Table of Contents
ToggleCashless Health Claim Process: A Complete Guide to Smooth & Hassle-Free Claim Settlement
What is a Cashless Health Claim?
Cashless health claim process allows policyholders to receive treatment at a network hospital without paying cash. The insurer settles the hospital bill provided that the treatment is received at a network hospital (a hospital with which the insurance company has an understanding).
Cashless Health Claim Process In simple terms: you get the treatment and the hospital sends the bill to your insurer. You only pay for the things that your policy does not cover.
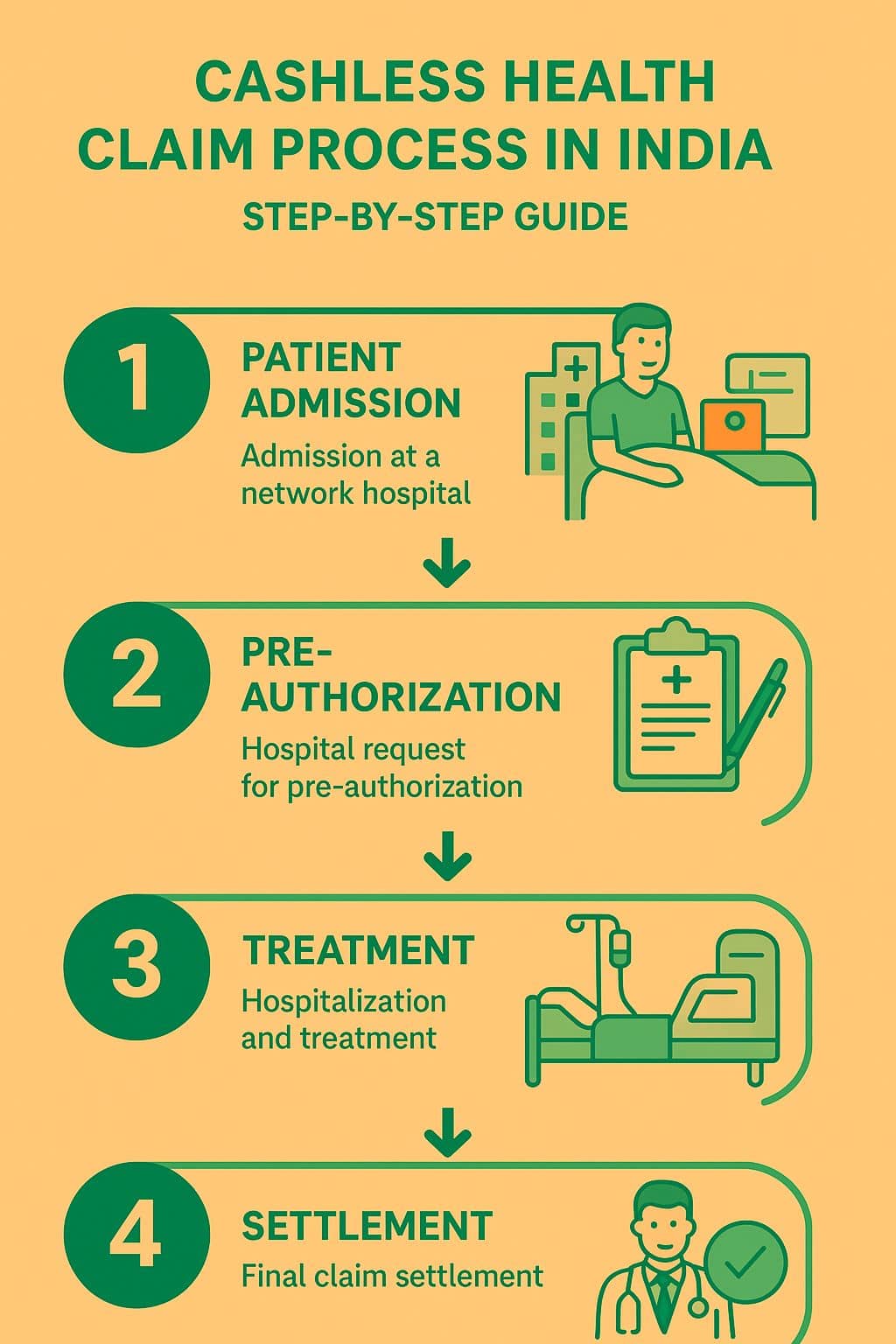
Step-by-Step Cashless Claim Procedure in India – 2025
1. Admission at a Network Hospital
Select a hospital from your insurance company’s network hospital list.
Show your health insurance card and a valid photo identification at the hospital counter.
The hospital cross-checks your policy details with the insurer or TPA (Third-Party Administrator).
2. Pre-Authorization Request
The hospital submits a pre-authorization form to the insurer/TPA.
This consists of the diagnosis, estimated cost of treatment, and doctor’s recommendations.
Once verified, the insurer issues an initial approval for the claim.
3. Hospitalization and Treatment
You undergo treatment without paying upfront.
Do note: non-medical expenses (like food, luxury rooms, or personal convenience items) may not be covered, and you’ll need to bear them.
4. Claim Processing During Stay
The insurer/TPA monitors bills and treatment progress.
If the insurer raises queries, the hospital coordinates for clarifications.
In the event of partial rejection or approval, you might have to pay and submit a claim for reimbursement afterward.
5. Final Settlement on Discharge
Post-discharge, final bills and reports are dispatched by the hospital to the insurer.
The insurer checks the claim against policy conditions.
The settled amount of the approved claim is remitted directly to the hospital.
You only have to settle non-covered charges prior to discharge.
Documents Necessary for Cashless Claims
Have the following documents in order for hassle-free processing:
Health insurance card / e-card
Aadhaar or government ID proof
Doctor’s prescription & diagnostic reports
Pre-authorization form (hospital-filled)
Discharge summary & final hospital bill
Common Reasons for Claim Rejection
Certain claims might get rejected or delayed because of:
Treatment at a non-network hospital
Pre-existing ailments not covered under the policy
Incomplete or incorrect documentation
Charges more than policy limits or sub-limits
Tip: Always read your policy with care and clear your doubts with your insurer before emergencies crop up.
Advantages of Cashless Health Claim Facility
No advance payment at the time of hospitalization
Convenience and hassle-free settlement between insurer and hospital
Rapid approvals by TPAs and insurer helplines
Relief of mind in case of emergency or pre-planned treatment
Tips for a Seamless Cashless Claim in 2025
Make sure your hospital is listed in the network.
Always keep your insurance card and valid ID with you.
Ensure that documentation is accurate and complete.
Maintain a relationship with the insurer’s customer support at the time of admission.
Check your policy conditions for exclusions and sub-limits.
Final Thoughts
India’s cashless health claim process (2025) is intended to make health care and hassle-free. Knowing the step-by-step process, documents required, and potential difficulties involved, you can have a smooth claim process.
Equipping yourself with a suitable health insurance plan not only safeguards your wallet but also promises prompt treatment without any fear of hospital expenses.
???? Keep in mind: In a crisis, being informed can save time and anxiety.
6. Conclusion
The cashless health claim process is one of the most valuable aspects of contemporary health insurance in India. It helps policyholders to get good medical care at network hospitals without being pained by finding funds in case of emergencies. Following the step-by-step process, having all necessary documents available, and knowledge of frequent grounds for claim rejection will make the process hassle-free and tension-free.
By 2025, cashless claims are quicker, more transparent, and well-accepted everywhere in the hospital—healthcare has never been more accessible. Selecting the appropriate health insurance policy and being well-informed about your policy conditions will not just save time but bring much-needed peace of mind at the times when you need it most.
FREQUENTLY ASKED QUESTIONS?
❓ What is a cashless health claim?
A cashless health claim is a process where the hospital bills are directly settled between your health insurance company and the hospital. You don’t need to pay upfront, except for non-covered expenses.
❓ How does the cashless health claim process work?
The process involves choosing a network hospital, showing your health insurance card, the hospital sending a pre-authorization request to the insurer, and upon approval, the bills are settled directly between the insurer and hospital.
❓ Which documents are required for a cashless claim?
You usually need your health insurance card, ID proof, doctor’s prescription, and medical reports. The hospital may also ask for claim forms or treatment-related documents.
❓ Why can a cashless claim be rejected?
Claims can be rejected if treatment is taken at a non-network hospital, if the illness isn’t covered under your policy, if documents are missing, or if there’s a delay in notifying the insurer.
❓ How can I ensure a smooth cashless claim settlement?
Always choose network hospitals, keep all required documents ready, inform your insurer in time, and understand the exclusions in your policy to avoid surprises.